Congratulations to 4th year MLS student Emily Gates who was recently awarded a Johns Hopkins Tuition Subsidy Scholarships for the 2020-2021 academic year. Over the course of her tenure at Stevenson University, Emily has been .
Medical Laboratory Science News
Program Coordinator and Professor
Posts

Sunday, April 19 marks the beginning of Medical Laboratory Professionals Week, or put more simply, Lab Week.This year's Lab Week comes at an unprecedented time in history, when healthcare professionals in Maryland, throughout.

Mary Moorhouse (MLS ’07), Manager of the Blood and Tissue Banks at Sinai and Northwest Hospitals and Melissa Fisher (MLS ’17), Blood Bank, Sinai Hospital are making a difference for those infected with COVID-19. The Sinai.

A 16-year-old female presents to the hospital with a burning sensation in her leg. There is a noted ulcer that she has been trying to alleviate with antibiotics.
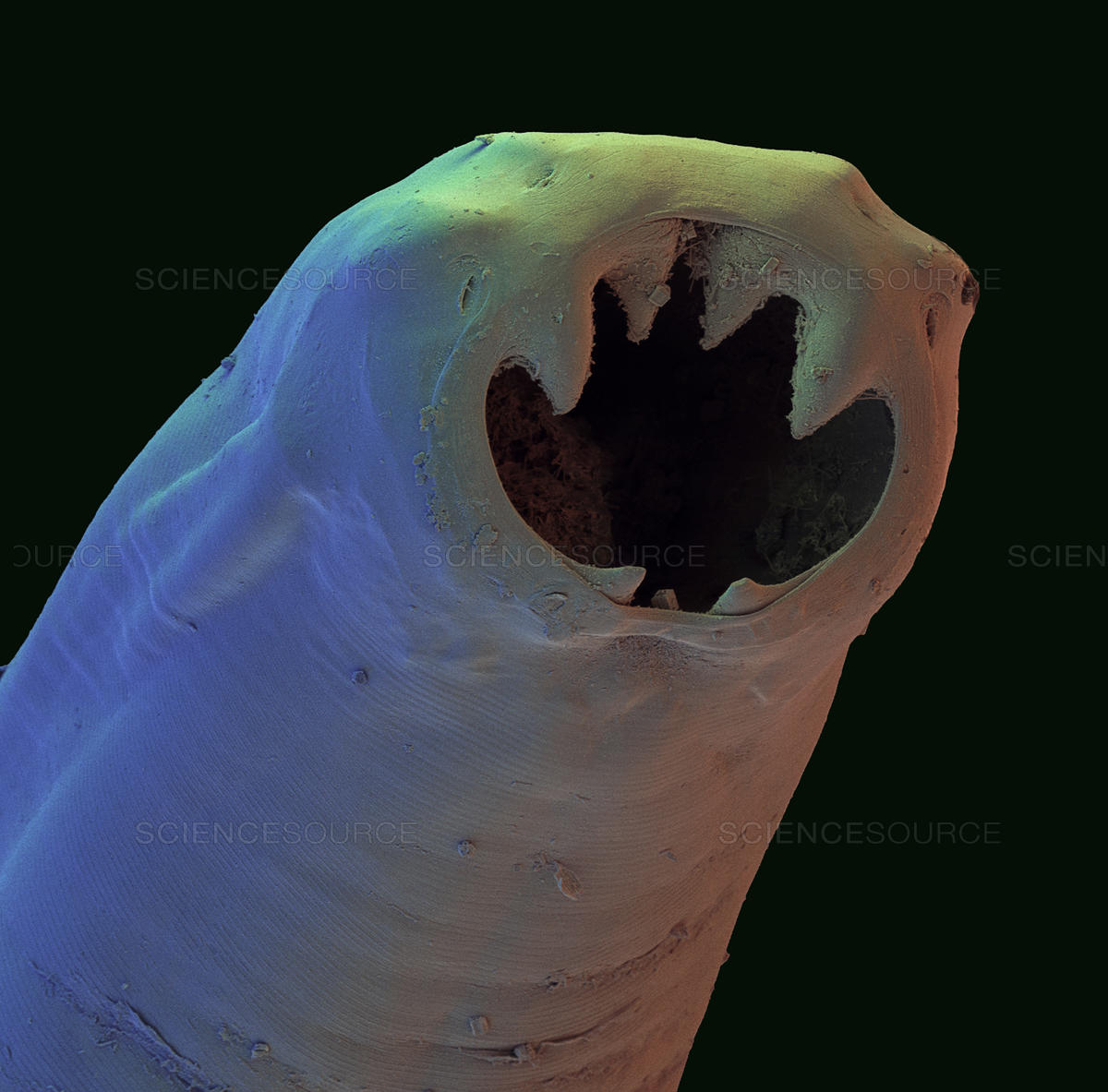
Human infection with parasitic worms can be devastating. Over a quarter of all humans are infected by parasites.